He has experience with both national and international athletes and recently transitioned to focusing primarily on helping the general population, and local athletes manage their pain and achieve their goals.
Listen: You need to listen before you begin to educate your patient. If you listen, you'll know everything that you need to address. You'll know what the patient's goal is, and you can take that information and apply it to them.
With listening, we'll know what they're looking for, expecting, and what makes them fearful. Only then can we can reassure our patients.
Reflective Listening: Reflect what they're saying, so they can either correct us or agree with us. There needs to be a sense of collaboration.
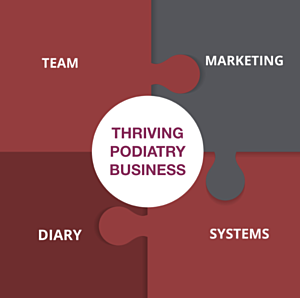
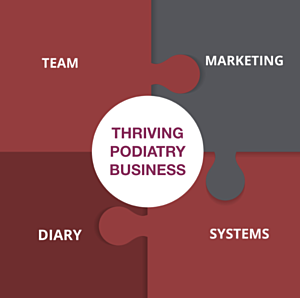
If you want to own and operate a Thriving Podiatry Business, there are four vital pieces to the business puzzle.
- Marketing - You need a well thought out marketing strategy, not just more tactics.
- Systems - You need systems that will support your marketing strategy and your team.
- Team - You need to develop a team culture that makes your work-life balance easier, not harder.
- Diary - Your diary needs to be structured in a way that maximises patient numbers and increases daily profits.
You have two choices: There's the slow approach, where you learn by trial and error and do everything yourself, or you can fast-track your education and business success with one-on-one business coaching and mentoring, or group coaching.
If you want to know more, please email me at tf@tysonfranklin.com, and we can set up a Zoom Call and have a quick chat to see if I can be of assistance.
ALEX'S REFERENCES
THE ESSENTIAL PAIN PAPER
Moseley, G. L. (2007). Reconceptualising pain according to modern pain science. Physical Therapy Reviews, 12(3), 169-178. doi: 10.1179/108331907X223010
Pain papers:
Atlas, L. Y., & Wager, T. D. (2012). How expectations shape pain. Neuroscience Letters, 520(2), 140-148. doi: https://doi.org/10.1016/j.neulet.2012.03.039
Hainline, B., Turner, J. A., Caneiro, J. P., Stewart, M., & Lorimer Moseley, G. (2017). Pain in elite athletes—neurophysiological, biomechanical and psychosocial considerations: a narrative review. Br J Sports Med, 51(17), 1259-1264. doi: 10.1136/bjsports-2017-097890
Harvie, D. S., Broecker, M., Smith, R. T., Meulders, A., Madden, V. J., & Moseley, G. L. (2015). Bogus visual feedback alters onset of movement-evoked pain in people with neck pain. Psychol Sci, 26(4), 385-392. doi: 10.1177/0956797614563339
Rio, E., Moseley, L., Purdam, C., Samiric, T., Kidgell, D., Pearce, A. J., . . . Cook, J. (2014). The pain of tendinopathy: physiological or pathophysiological? Sports Med, 44(1), 9-23. doi: 10.1007/s40279-013-0096-z
Testa, M., & Rossettini, G. (2016). Enhance placebo, avoid nocebo: How contextual factors affect physiotherapy outcomes. Man Ther, 24, 65-74. doi: 10.1016/j.math.2016.04.006
Understanding complexity/complex systems theory:
Bittencourt, N. F. N., Meeuwisse, W. H., Mendonça, L. D., Nettel-Aguirre, A., Ocarino, J. M., & Fonseca, S. T. (2016). Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. Br J Sports Med, 50(21), 1309-1314. doi: 10.1136/bjsports-2015-095850
Stern, B. D., Hegedus, E. J., & Lai, Y. C. (2020). Injury prediction as a non-linear system. Phys Ther Sport, 41, 43-48. doi: 10.1016/j.ptsp.2019.10.010
Biopsychosocial model of health
Engel, G. L. (1977). The need for a new medical model: a challenge for biomedicine. Science, 196(4286), 129-136. doi: 10.1126/science.847460
Engel, G. L. (1980). The clinical application of the biopsychosocial model. Am J Psychiatry, 137(5), 535-544. doi: 10.1176/ajp.137.5.535
Muscloskeletal Pain/Injury:
Caneiro, J. P., Roos, E. M., Barton, C. J., O'Sullivan, K., Kent, P., Lin, I., . . . O'Sullivan, P. (2020). It is time to move beyond ‘body region silos’ to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med, 54(8), 438-439. doi: 10.1136/bjsports-2018-100488
Lewis, J., & O’Sullivan, P. (2018). Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med, 52(24), 1543-1544. doi: 10.1136/bjsports-2018-099198
Lin, I., Wiles, L., Waller, R., Goucke, R., Nagree, Y., Gibberd, M., . . . O’Sullivan, P. P. B. (2020). What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med, 54(2), 79-86. doi: 10.1136/bjsports-2018-099878
Shared Decision Making:
Hoffmann, T. C., Lewis, J., & Maher, C. G. (2020). Shared decision making should be an integral part of physiotherapy practice. Physiotherapy, 107, 43-49. doi: https://doi.org/10.1016/j.physio.2019.08.012
Clinical Decision Making:
Simpkin, A. L., & Schwartzstein, R. M. (2016). Tolerating Uncertainty - The Next Medical Revolution? N Engl J Med, 375(18), 1713-1715. doi: 10.1056/NEJMp1606402
Walton, D. M. (2019). The critical skill of asking why? An endorsement of critical reflection in physiotherapy research and practice. Musculoskelet Sci Pract, 41, iv-v. doi: 10.1016/j.msksp.2019.04.005
Zou, K., Wong, J., Abdullah, N., Chen, X., Smith, T., Doherty, M., & Zhang, W. (2016). Examination of overall treatment effect and the proportion attributable to contextual effect in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis, 75(11), 1964-1970. doi: 10.1136/annrheumdis-2015-208387
Communication:
Soklaridis, S., Hunter, J. J., & Ravitz, P. (2014). Twelve tips for asking and responding to difficult questions during a challenging clinical encounter. Med Teach, 36(9), 769-774. doi: 10.3109/0142159x.2014.916782
Zolnierek, K. B. H., & Dimatteo, M. R. (2009). Physician communication and patient adherence to treatment: a meta-analysis. Medical care, 47(8), 826-834. doi: 10.1097/MLR.0b013e31819a5acc